Anatomy of Shin Splints: Treatment and Prevention

Shin Splints Treatment and Prevention – read about this uncomfortable exercise issue.
Shin splints are a common exercise-related problem. The term “shin splints” refers to pain along the inner edge of the shinbone (tibia).
Shin splints typically develop after physical activity. They are often associated with running. Any vigorous sports activity can bring on shin splints, especially if you are just starting a fitness program.
Simple measures can relieve the pain of shin splints. Rest, ice, and stretching often help. Taking care not to overdo your exercise routine will help prevent shin splints from coming back.
Description
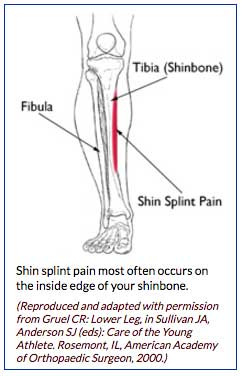
Shin splints (medial tibial stress syndrome) is an inflammation of the muscles, tendons, and bone tissue around your tibia. Pain typically occurs along the inner border of the tibia, where muscles attach to the bone.
(Reproduced and adapted with permission from Gruel CR: Lower Leg, in Sullivan JA, Anderson SJ (eds): Care of the Young Athlete. Rosemont, IL, American Academy of Orthopaedic Surgeon, 2000.)
Cause
In general, shin splints develop when the muscle and bone tissue (periosteum) in the leg become overworked by repetitive activity.
Shin splints often occur after sudden changes in physical activity. These can be changes in frequency, such as increasing the number of days you exercise each week. Changes in duration and intensity, such as running longer distances or on hills, can also cause shin splints.
Other factors that contribute to shin splints include:
- Having flat feet or abnormally rigid arches
- Exercising with improper or worn-out footwear
Runners are at highest risk for developing shin splints. Dancers and military recruits are two other groups frequently diagnosed with the condition.
Symptoms:
The most common symptom of shin splints is pain along the border of the tibia. Mild swelling in the area may also occur.
Shin splint pain may:
- Be sharp and razor-like or dull and throbbing
- Occur both during and after exercise
- Be aggravated by touching the sore spot
Doctor Examination
After discussing your symptoms and medical history, your doctor will examine your lower leg. An accurate diagnosis is very important. Sometimes, other problems may exist that can have an impact on healing.
Your doctor may order additional imaging tests to rule out other shin problems. Several conditions can cause shin pain, including stress fractures, tendinitis, and chronic exertional compartment syndrome.
Stress Fracture
If your shin splints are not responsive to treatment, your doctor may want to make sure you do not have a stress fracture. A stress fracture is a small crack(s) in the tibia caused by stress and overuse.
Imaging tests that create pictures of anatomy help to diagnose conditions. A bone scan and magnetic resonance imaging (MRI) study will often show stress fractures in the tibia.
Tendinitis
Tendons attach muscles to bones. Tendinitis occurs when tendons become inflamed. This can be painful like shin splints, especially if there is a partial tear of the involved tendon. An MRI can help diagnose tendinitis.
Chronic Exertional Compartment Syndrome
An uncommon condition called chronic exertional compartment syndrome causes symptoms like shin splints. Compartment syndrome is a painful condition that occurs when pressure within the muscles builds to dangerous levels. In chronic exertional compartment syndrome, this is brought on by exercise. Pain usually resolves soon after the activity stops.
The tests used to diagnose this condition involve measuring the pressure within the leg compartments before and after exercise.
Treatment
Nonsurgical Treatment
- Rest. Because shin splints are typically caused by overuse, standard treatment includes several weeks of rest from the activity that caused the pain. Lower impact types of aerobic activity can be substituted during your recovery, such as swimming, using a stationary bike, or an elliptical trainer.
- Non-steroidal anti-inflammatory medicines. Drugs like ibuprofen, aspirin, and naproxen reduce pain and swelling.
- Ice. Use cold packs for 20 minutes at a time, several times a day. Do not apply ice directly to the skin.
- Compression. Wearing an elastic compression bandage may prevent additional swelling.
- Flexibility exercises. Stretching your lower leg muscles may make your shins feel better.
- Supportive shoes. Wearing shoes with good cushioning during daily activities will help reduce stress in your shins.
- Orthotics. People who have flat feet or recurrent problems with shin splints may benefit from orthotics. Shoe inserts can help align and stablize your foot and ankle, taking stress off of your lower leg. Orthotics can be custom-made for your foot, or purchased “off the shelf.”
- Return to exercise. Shin splints usually resolve with rest and the simple treatments described above. Before returning to exercise, you should be pain-free for at least 2 weeks. Keep in mind that when you return to exercise, it must be at a lower level of intensity. You should not be exercising as often as you did before, or for the same length of time.
Be sure to warm up and stretch thoroughly before you exercise. Increase training slowly. If you start to feel the same pain, stop exercising immediately. Use a cold pack and rest for a day or two. Return to training again at a lower level of intensity. Increase training even more slowly than before.
Surgical Treatment
Very few people need surgery for shin splints. Surgery has been done in very severe cases that do not respond to nonsurgical treatment. It is not clear how effective surgery is, however.
Prevention
There are things you can do to prevent shin splints.
Wear a proper fitting athletic shoe. To get the right fit, determine the shape of your foot using the “wet test.” Step out of the shower onto a surface that will show your footprint, like a brown paper bag. If you have a flat foot, you will see an impression of your whole foot on the paper. If you have a high arch, you will only see the ball and heel of your foot. When shopping, look for athletic shoes that match your particular foot pattern.
In addition, make sure you wear shoes designed for your sport. Running long distances in court-type sneakers can contribute to shin splints.
Slowly build your fitness level. Increase the duration, intensity, and frequency of your exercise regimen gradually.
Cross train. Alternate jogging with lower impact sports like swimming or cycling.
Barefoot running. In recent years, barefoot running has gained in popularity. Many people claim it has helped to resolve shin splints. Some research indicates that barefoot running spreads out impact stresses among muscles, so that no area is overloaded. However, there is no clear evidence that barefoot running reduces the risk for any injury.
Like any significant change in your fitness regimen, a barefoot running program should be started very gradually. Begin with short distances to give your muscles and your feet time to adjust. Pushing too far, too fast can put you at risk for stress injuries. In addition, barefoot runners are at increased risk for cuts and bruises on their feet. Several brands of minimalist shoes with “toes” are available and these also require a slow working in period as your body adjusts to this different activity.
If your shin splints do not improve after rest and other methods described above, be sure to see a doctor to determine whether something else is causing your leg pain.
BoulderCentre can help. Call us (303) 449-2730 and ask to see one of our foot and ankle specialists or choose from any one of our many surgical or general health practitioners.
Article courtesy of AAOS: American Academy of Orthopedic Surgeons.





