Achilles Tendinitis
Achilles tendinitis is a common condition that causes pain along the back of the leg near the heel.
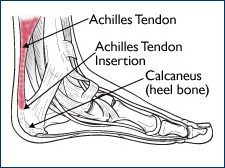
The Achilles tendon is the largest tendon in the body. It connects your calf muscles to your heel bone and is used when you walk, run, and jump.
Although the Achilles tendon can withstand great stresses from running and jumping, it is also prone to tendinitis, a condition associated with overuse and degeneration.
Description
Simply defined, tendinitis is inflammation of a tendon. Inflammation is the body’s natural response to injury or disease, and often causes swelling, pain, or irritation. There are two types of Achilles tendinitis, based upon which part of the tendon is inflamed.
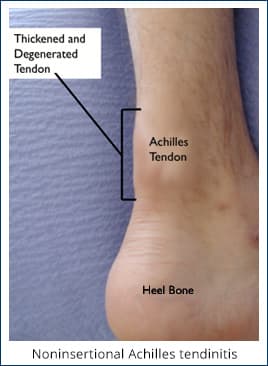
Noninsertional Achilles Tendinitis
In noninsertional Achilles tendinitis, fibers in the middle portion of the tendon have begun to break down with tiny tears (degenerate), swell, and thicken.
Tendinitis of the middle portion of the tendon more commonly affects younger, active people.
Insertional Achilles Tendinitis
Insertional Achilles tendinitis involves the lower portion of the heel, where the tendon attaches (inserts) to the heel bone.
In both noninsertional and insertional Achilles tendinitis, damaged tendon fibers may also calcify (harden). Bone spurs (extra bone growth) often form with insertional Achilles tendinitis.
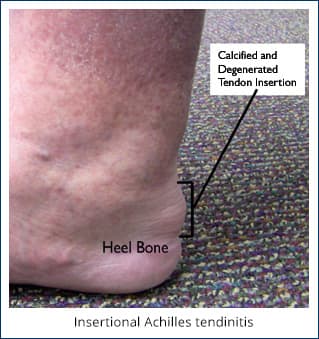 Tendinitis that affects the insertion of the tendon can occur at any time, even in patients who are not active.
Tendinitis that affects the insertion of the tendon can occur at any time, even in patients who are not active.
Cause
Achilles tendinitis is typically not related to a specific injury. The problem results from repetitive stress to the tendon. This often happens when we push our bodies to do too much, too soon, but other factors can make it more likely to develop tendinitis, including:
- Sudden increase in the amount or intensity of exercise activity—for example, increasing the distance you run every day by a few miles without giving your body a chance to adjust to the new distance
- Tight calf muscles—Having tight calf muscles and suddenly starting an aggressive exercise program can put extra stress on the Achilles tendon
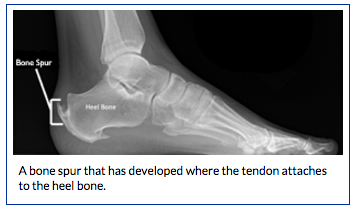
- Bone spur—Extra bone growth where the Achilles tendon attaches to the heel bone can rub against the tendon and cause pain
Symptoms
 Common symptoms of Achilles tendinitis include:
Common symptoms of Achilles tendinitis include:
- Pain and stiffness along the Achilles tendon in the morning
- Pain along the tendon or back of the heel that worsens with activity
- Severe pain the day after exercising
- Thickening of the tendon
- Bone spur (insertional tendinitis)
- Swelling that is present all the time and gets worse throughout the day with activity
If you have experienced a sudden “pop” in the back of your calf or heel, you may have ruptured (torn) your Achilles tendon. See your doctor immediately if you think you may have torn your tendon.
Doctor Examination
After you describe your symptoms and discuss your concerns, the doctor will examine your foot and ankle. The doctor will look for these signs:
- Swelling along the Achilles tendon or at the back of your heel
- Thickening or enlargement of the Achilles tendon
- Bony spurs at the lower part of the tendon at the back of your heel (insertional tendinitis)
- The point of maximum tenderness
- Pain in the middle of the tendon, (noninsertional tendinitis)
- Pain at the back of your heel at the lower part of the tendon (insertional tendinitis)
- Limited range of motion in your ankle—specifically, a decreased ability to flex your foot
Tests
Your doctor may order imaging tests to make sure your symptoms are caused by Achilles tendinitis.
X-rays
X-ray tests provide clear images of bones. X-rays can show whether the lower part of the Achilles tendon has calcified, or become hardened. This calcification indicates insertional Achilles tendinitis. In cases of severe noninsertional Achilles tendinitis, there can be calcification in the middle portion of the tendon, as well.
Magnetic Resonance Imaging (MRI)
Although magnetic resonance imaging (MRI) is not necessary to diagnose Achilles tendinitis, it is important for planning surgery. An MRI scan can show how severe the damage is in the tendon. If surgery is needed, your doctor will select the procedure based on the amount of tendon damage.
Treatment
Nonsurgical Treatment
In most cases, nonsurgical treatment options will provide pain relief, although it may take a few months for symptoms to completely subside. Even with early treatment, the pain may last longer than 3 months. If you have had pain for several months before seeking treatment, it may take 6 months before treatment methods take effect.
Rest. The first step in reducing pain is to decrease or even stop the activities that make the pain worse. If you regularly do high-impact exercises (such as running), switching to low-impact activities will put less stress on the Achilles tendon. Cross-training activities such as biking, elliptical exercise, and swimming are low-impact options to help you stay active.
Ice. Placing ice on the most painful area of the Achilles tendon is helpful and can be done as needed throughout the day. This can be done for up to 20 minutes and should be stopped earlier if the skin becomes numb. A foam cup filled with water and then frozen creates a simple, reusable ice pack. After the water has frozen in the cup, tear off the rim of the cup. Then rub the ice on the Achilles tendon. With repeated use, a groove that fits the Achilles tendon will appear, creating a “custom-fit” ice pack.
Non-steroidal anti-inflammatory medication. Drugs such as ibuprofen and naproxen reduce pain and swelling. They do not, however, reduce the thickening of the degenerated tendon. Using the medication for more than 1 month should be reviewed with your primary care doctor.
Exercise. The following exercise can help to strengthen the calf muscles and reduce stress on the Achilles tendon.
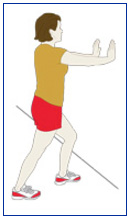 Calf stretch. Lean forward against a wall with one knee straight and the heel on the ground. Place the other leg in front, with the knee bent. To stretch the calf muscles and the heel cord, push your hips toward the wall in a controlled fashion. Hold the position for 10 seconds and relax. Repeat this exercise 20 times for each foot. A strong pull in the calf should be felt during the stretch.
Calf stretch. Lean forward against a wall with one knee straight and the heel on the ground. Place the other leg in front, with the knee bent. To stretch the calf muscles and the heel cord, push your hips toward the wall in a controlled fashion. Hold the position for 10 seconds and relax. Repeat this exercise 20 times for each foot. A strong pull in the calf should be felt during the stretch.- Physical Therapy. Physical therapy is very helpful in treating Achilles tendinitis. It has proven to work better for noninsertional tendinitis than for insertional tendinitis.
- Eccentric Strengthening Protocol. Eccentric strengthening is defined as contracting (tightening) a muscle while it is getting longer. Eccentric strengthening exercises can cause damage to the Achilles tendon if they are not done correctly. At first, they should be performed under the supervision of a physical therapist. Once mastered with a therapist, the exercises can then be done at home. These exercises may cause some discomfort, however, it should not be unbearable.
 Bilateral heel drop. Stand at the edge of a stair, or a raised platform that is stable, with just the front half of your foot on the stair. This position will allow your heel to move up and down without hitting the stair. Care must be taken to ensure that you are balanced correctly to prevent falling and injury. Be sure to hold onto a railing to help you balance.
Bilateral heel drop. Stand at the edge of a stair, or a raised platform that is stable, with just the front half of your foot on the stair. This position will allow your heel to move up and down without hitting the stair. Care must be taken to ensure that you are balanced correctly to prevent falling and injury. Be sure to hold onto a railing to help you balance.
Lift your heels off the ground then slowly lower your heels to the lowest point possible. Repeat this step 20 times. This exercise should be done in a slow, controlled fashion. Rapid movement can create the risk of damage to the tendon. As the pain improves, you can increase the difficulty level of the exercise by holding a small weight in each hand.
- Single leg heel drop. This exercise is performed similarly to the bilateral heel drop, except that all your weight is focused on one leg. This should be done only after the bilateral heel drop has been mastered.
Cortisone injections. Cortisone, a type of steroid, is a powerful anti-inflammatory medication. Cortisone injections into the Achilles tendon are rarely recommended because they can cause the tendon to rupture (tear).
Supportive shoes and orthotics. Pain from insertional Achilles tendinitis is often helped by certain shoes, as well as orthotic devices. For example, shoes that are softer at the back of the heel can reduce irritation of the tendon. In addition, heel lifts can take some strain off the tendon.
Heel lifts are also very helpful for patients with insertional tendinitis because they can move the heel away from the back of the shoe, where rubbing can occur. They also take some strain off the tendon. Like a heel lift, a silicone Achilles sleeve can reduce irritation from the back of a shoe.
If your pain is severe, your doctor may recommend a walking boot for a short time. This gives the tendon a chance to rest before any therapy is begun. Extended use of a boot is discouraged, though, because it can weaken your calf muscle.
Extracorporeal shockwave therapy (ESWT). During this procedure, high-energy shockwave impulses stimulate the healing process in damaged tendon tissue. ESWT has not shown consistent results and, therefore, is not commonly performed.
ESWT is noninvasive—it does not require a surgical incision. Because of the minimal risk involved, ESWT is sometimes tried before surgery is considered.
Surgical Treatment
Surgery should be considered to relieve Achilles tendinitis only if the pain does not improve after 6 months of nonsurgical treatment. The specific type of surgery depends on the location of the tendinitis and the amount of damage to the tendon.
Gastrocnemius recession. This is a surgical lengthening of the calf (gastrocnemius) muscles. Because tight calf muscles place increased stress on the Achilles tendon, this procedure is useful for patients who still have difficulty flexing their feet, despite consistent stretching.
In gastrocnemius recession, one of the two muscles that make up the calf is lengthened to increase the motion of the ankle. The procedure can be performed with a traditional, open incision or with a smaller incision and an endoscope—an instrument that contains a small camera. Your doctor will discuss the procedure that best meets your needs.
Complication rates for gastrocnemius recession are low, but can include nerve damage.
Gastrocnemius recession can be performed with or without débridement, which is removal of damaged tissue.
Débridement and repair (tendon has less than 50% damage). The goal of this operation is to remove the damaged part of the Achilles tendon. Once the unhealthy portion of the tendon has been removed, the remaining tendon is repaired with sutures, or stitches to complete the repair.
In insertional tendinitis, the bone spur is also removed. Repair of the tendon in these instances may require the use of metal or plastic anchors to help hold the Achilles tendon to the heel bone, where it attaches.
After débridement and repair, most patients are allowed to walk in a removable boot or cast within 2 weeks, although this period depends upon the amount of damage to the tendon.
Débridement with tendon transfer (tendon has greater than 50% damage). In cases where more than 50% of the Achilles tendon is not healthy and requires removal, the remaining portion of the tendon is not strong enough to function alone. To prevent the remaining tendon from rupturing with activity, an Achilles tendon transfer is performed. The tendon that helps the big toe point down is moved to the heel bone to add strength to the damaged tendon. Although this sounds severe, the big toe will still be able to move, and most patients will not notice a change in the way they walk or run.
Depending on the extent of damage to the tendon, some patients may not be able to return to competitive sports or running.
Recovery. Most patients have good results from surgery. The main factor in surgical recovery is the amount of damage to the tendon. The greater the amount of tendon involved, the longer the recovery period, and the less likely a patient will be able to return to sports activity.
Physical therapy is an important part of recovery. Many patients require 12 months of rehabilitation before they are pain-free.
Complications. Moderate to severe pain after surgery is noted in 20% to 30% of patients and is the most common complication. In addition, a wound infection can occur and the infection is very difficult to treat in this location.
BoulderCentre can help. Call us (303) 449-2730 and ask to see one of our foot and ankle specialists or choose from any one of our sports medicine specialists.
Article courtesy of AAOS: American Academy of Orthopaedic Surgeons.